Background: Shared Decision Making (SDM) is a core component of facilitating patient-centered care. When implementing SDM, patients, parents and clinicians make health decisions together, ensuring that families are informed to make decisions based on their values and preferences. This is of particular importance among children and adolescents with chronic conditions, who are often presented with health-related decisions that can have social and psychological implications. Despite increasing recommendations for use of SDM tools, evidence-based recommendations regarding their use in clinical practice are limited. Studies suggest that barriers to SDM implementation include poor quality of information tailored to children and their families, the emotional state of the patients and their families (denial, anxious, overwhelmed, etc.), power imbalance with health care providers, and insufficient time from heavy physicians' workloads. Due to its limited implementation in clinical practice, little is known about proper approaches and outcomes of SDM tools among children and adolescents with chronic conditions.
Objectives: To evaluate and summarize the literature related to how SDM tools are being studied and implemented children and adolescents with chronic medical conditions and how they influence decision making and health outcomes.
Methods: A literature search was conducted for publications written in English from 2013-2023 using PubMed, MEDLINE, and Google Scholar. Search terms included “shared decision making”, “decision aid,” “pediatrics,” “infant,” “child,” “adolescents,” and “chronic conditions” to ensure adequate representation of the available literature. Relevant articles included those that covering SDM in hematological and non-hematological chronic conditions in pediatrics.
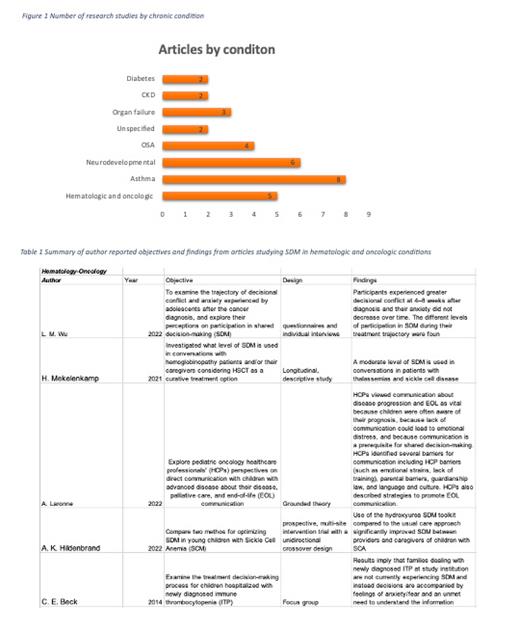
Results: Out of 171 studies identified through literature search, 35 were included. Areas in which SDM has been most studied included hematologic and oncologic conditions (n=5), asthma (n=8), autism, other neurodevelopmental disorders (n=6), Obstructive Sleep Apnea (n=4), inflammatory bowel disease (n=1), chronic kidney disease (n=2), and diabetes (n=2), organ failure (n=3), and other conditions (n=4). Of those, 20 studies were descriptive and 15 had an experimental intervention design. Only 4 studies focused on the child's role in SDM while others focused on parent or caregiver role. Implementation of SDM toolkits and patient portals help decrease asthma exacerbations and emergency room visits. Similar toolkits and decision aids developed for decision making in hematologic and respiratory disease have shown reduced decisional conflict regarding treatment choice. In contrast, researched tools developed for diabetes patients did not show improved outcomes but did reduce decisional conflict. Results demonstrate that although patient with greatest functional neurodevelopmental impairment experience less SDM, its use leads to significant improvements in severity of their condition, behavioral, and psychoeducational levels. Research on hematological conditions such as sickle cell, thalassemia, and immune thrombocytopenia all show that their patients are not experiencing SDM, or it's limited to moderate amounts. Both children and parents desire to become more active members of the decision-making progress. Perspective of physicians show that they understand this desire but face barriers such as poor quality of available information, lack of time, or the family's emotional state. Effective training tools are being studied to help enhance SDM care and overcome these obstacles.
Conclusions: There is limited evidence for the implementation of pediatric-focused SDM tools in hematological and non-hematological chronic conditions. Published studies in pediatrics have been mostly descriptive and have placed little emphasis on implementation and effectiveness of shared decision-making interventions. Barriers and facilitators to SDM have been explored, but a gap in knowledge still exists regarding the proven methods for SDM. In general, available studies showed benefit in patients' health outcomes, satisfaction with decision making, and treatment adherence. Future research should involve the implementation of patient-centered SDM aids in efforts to overcome known barriers and to establish evidence-based guidelines for their use.
Disclosures
Badawy:Forma Therapeutics/Novo Nordisk: Consultancy; Editas Medicine: Consultancy; Vertex Pharmaceuticals Inc: Consultancy; Bluebird bio, INC: Consultancy; Bristol-Myers Squibb: Consultancy; GBT/Pfizer: Consultancy; Chiesi, Inc: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal